“We were all hard-working men … and citizens of the United States.”
Herman Shaw, 1997
Born in Alabama in 1902, Herman Shaw was a farmer and a cotton mill worker. He and his wife, Fannie Mae, were married for 62 years and had two children and six grandchildren.
Shaw was also a survivor of a 40-year medical experiment.
From 1932 until the Associated Press broke the story in 1972, the U.S. Public Health Service conducted a study of more than 600 Black men in Macon County, Ala., without their informed consent. The men were told they were being tested and receiving free therapies for “bad blood,” a local term for several ailments. Instead, it was a study of untreated syphilis. Roughly two-thirds of the men had the transmissible disease. The Public Health Service did not disclose to the men their diagnoses and withheld available treatments.
Science News headlines, in your inbox
Headlines and summaries of the latest Science News articles, delivered to your email inbox every Friday.
Client key* E-mail Address* Sign up
Thank you for signing up!
There was a problem signing you up.
The experiment tracked the damage the disease inflicted on the men. The endpoint was death.
In the 50 years since its end, the U.S. Public Health Service Study of Untreated Syphilis at Tuskegee in Alabama has often been held up as a primary driver of distrust of the U.S. health care system in Black communities. Yet medical abuse of Black people has occurred throughout U.S. history.
White people have long justified abuse and mistreatment of Black people by describing them, explicitly and implicitly, as inferior. There have been “four hundred years of active decisions to dehumanize Black people and Black bodies,” says Rachel Hardeman, a reproductive health equity researcher at the University of Minnesota School of Public Health in Minneapolis.
As John Heller, chief of the Division of Venereal Diseases at the U.S. Public Health Service from 1943 to 1948, did. Heller said in an interview with historian James Jones for his book on the syphilis study, “Bad Blood,” that “the men’s status did not warrant ethical debate. They were subjects, not patients; clinical material, not sick people.”
Half a century later, this racist experiment can look like a product of a long-gone era, even as it gets outsize credit for distrust today. In reality, the racism that fueled the syphilis study has existed for centuries and still permeates the U.S. health care system, causing racial disparities in access to medical care and measures of health. While there are a variety of efforts to address these disparities, including medical training to bring awareness of racial biases, there is far to go.
“It is never too late to work to restore faith and trust,” Herman Shaw said in 1997 when the United States apologized for the study. U.S. President Joe Biden echoed these words during a November 30 event acknowledging the 50th anniversary of the end of the study: “Restoring faith and trust is the work of our time.”
Experimentation during slavery
“A slave is not a human being in the eye of the law, and the slaveholder looks upon him just as what the law makes him; nothing more, and perhaps even something less.”
John Brown, 1855
In his 1855 memoir, John Brown wrote about his enslavement in Georgia and his escape to England. He described being experimented on to test therapies for heat stroke. Brown was forced to sit in a fire-heated pit with only his head exposed.
“In about half an hour I fainted. I was then lifted out and revived, the doctor taking a note of the degree of heat when I left the pit,” Brown wrote. The experiments continued as the doctor investigated which medicine “enabled me to withstand the greatest degree of heat.”
The enslavement and abuse of Black Americans were sanctioned by prevailing medical theories. Antebellum doctors claimed that Black people “possessed peculiar physiological and anatomical features that justified their enslavement,” Vanessa Northington Gamble wrote in the American Journal of Preventive Medicine in 1993. “This medical distinctiveness, [the physicians] argued, made Africans not only inferior but inherently suited for slavery.” And for medical experimentation.
That included excruciatingly painful gynecological surgeries performed on enslaved Black women by white doctors, experiments that advanced the field. Thought of as biologically inferior to white women, while also deemed to have a high tolerance for pain, enslaved women were considered “perfect medical subjects” for experimentation, Deirdre Cooper Owens, a historian at the University of Nebraska–Lincoln, wrote in her 2017 book Medical Bondage: Race, Gender, and the Origins of American Gynecology.
 Artist Michelle Browder’s “Mothers of Gynecology” monument, unveiled in Montgomery, Ala., in 2021, depicts Anarcha, Betsy and Lucy, three enslaved Black women forced to undergo experimental gynecological surgeries in the 1840s. The experiments brought fame to surgeon J. Marion Sims, who became known as the “Father of Gynecology.”Steven Zucker/Flickr (CC BY-NC-SA 2.0)
Artist Michelle Browder’s “Mothers of Gynecology” monument, unveiled in Montgomery, Ala., in 2021, depicts Anarcha, Betsy and Lucy, three enslaved Black women forced to undergo experimental gynecological surgeries in the 1840s. The experiments brought fame to surgeon J. Marion Sims, who became known as the “Father of Gynecology.”Steven Zucker/Flickr (CC BY-NC-SA 2.0)
Anarcha, Betsy and Lucy were among about a dozen enslaved women who surgeon J. Marion Sims experimented on. He performed surgeries on the women, without anesthesia, to develop a repair for an abnormal opening between the bladder and the vagina. Held on Sims’ property from 1844 to 1849, the women were trained by Sims to assist with the procedure and became his surgical nurses, Cooper Owens wrote.
The work brought Sims renown as a gynecological surgeon. But, she wrote, “the central role that enslaved women played in these advances — by providing doctors the bodies and sometimes labor needed for experimentation, treatment, and repair — went unacknowledged.”
Embedded racism
“The Alabama community offered an unparalleled opportunity for the study of the effect of untreated syphilis.”
Taliaferro Clark, Public Health Service, 1932
In the early 20th century, white physicians attributed the high rates of syphilis among Black people to their supposed immorality and excessive sexual desire. White doctors alleged that the disease was difficult to treat in Black people, because they wouldn’t reliably seek out or follow a therapeutic regimen, Northington Gamble wrote in the American Journal of Preventive Medicine.
Another prevailing theory that motivated the experiment was “the belief that syphilis was a different disease in African Americans than it was in white people,” says Northington Gamble, a medical historian and physician at George Washington University in Washington, D.C. “This whole theory of Black bodies being fundamentally different was a foundation not only of the syphilis study, but also the foundation of medical practice.”
The idea persists today. Race is a social concept, but using race as though it designates biological differences informs treatment decisions about the kidneys, the lungs, pregnancy and more.
For example, an equation that estimates kidney function long included a race-based adjustment, despite a lack of evidence for its use. The adjustment could mask the kidneys’ true condition in Black people.
Without the adjustment, 3.3 million more Black Americans met a threshold for stage 3 chronic kidney disease, researchers reported in eClinicalMedicine in 2021. At this stage, complications from kidney disease start to occur, meaning Black Americans could be missing out on needed care, the researchers wrote. A new equation to estimate kidney function without a race adjustment is starting to be used in clinical practice.
In contrast, the belief that Black people experience less pain than white people hasn’t been extinguished. Today, Black people often report their pain is not taken seriously and evidence shows their pain is undertreated.
“Racism has been baked into health care,” Hardeman says. It’s embedded in the system: in therapeutic protocols, in the distribution of health care resources, in how a physician treats a patient (SN: 4/5/22).
Black people are nearly twice as likely as white people to have procedures during perinatal care and birth done without their consent, researchers reported in Birth in June. Hardeman has talked to Black people whose doctors sent their urine samples for toxicological screens in prenatal visits without their consent. “There’s this underlying assumption that there is likely drug use and that a tox screen is necessary,” she says.
Unequal outcomes
The maternal mortality rate for Black women is about three times the rate for white women and for Hispanic women, according to the U.S. Centers for Disease Control and Prevention. The latest data, from 2020, reports 55 deaths per 100,000 live births for Black women, compared with 19 per 100,000 for white women and 18 per 100,000 for Hispanic women.
U.S. maternal mortality rates by race and ethnicity, 2018–2020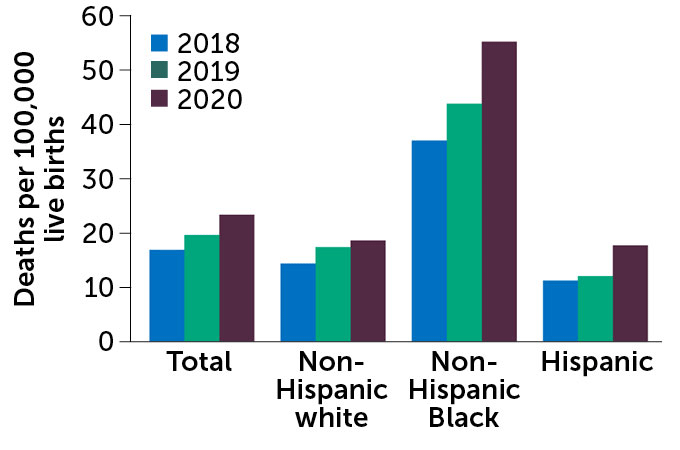 C. ChangC. Chang SOURCE: National Vital Statistics System, Mortality/National Center for Health Statistics
C. ChangC. Chang SOURCE: National Vital Statistics System, Mortality/National Center for Health Statistics
This embedded, structural racism is a risk to health, and underlies health disparities at birth and throughout life in the United States. Black newborns are more likely to die than white newborns (SN: 8/25/20). The rate of maternal mortality for Black women is nearly three times that of white women. Black people are more likely than white people to die early from diseases that are treatable with access to care.
Singling out the syphilis study when discussing African Americans’ attitudes towards the medical system is “overly simplistic and historically inaccurate,” Northington Gamble says. The view that “the medical profession did not always have the best interest of African Americans at heart predated the syphilis study.” And the burden shouldn’t be on African Americans to change their attitudes, she says. “Trust should be earned.”
Along with past examples, there are plenty of modern-day instances of medical racism that contribute to distrust, says Fatima Cody Stanford, an obesity medicine physician scientist at Massachusetts General Hospital and Harvard Medical School in Boston. “Every single day it’s still going on,” she says.
Beyond the syphilis study
“What the United States government did was shameful, and I am sorry.”
President Bill Clinton, 1997
Twenty-five years after the end of the syphilis study, the U.S. government apologized. Northington Gamble was part of the committee that helped to make the apology happen. She spoke about the event during the November 30 remembrance of the syphilis study, hosted by the U.S. Centers for Disease Control and Prevention in Atlanta.
“When President Clinton said, ‘and I am sorry,’ … there were sobs around the room,” Northington Gamble said. “And it wasn’t sobs just about the syphilis study, but it was sobs about how Black people have been treated in this country.”
 Herman Shaw introduced President Clinton (the two are shown embracing) when the U.S. government apologized for the syphilis study in May of 1997. “In order for America to reach its fullest potential, we must truly be one America … trusting each other, caring for each other,” Shaw said during his speech.STEPHEN JAFFE/AFP via Getty Images
Herman Shaw introduced President Clinton (the two are shown embracing) when the U.S. government apologized for the syphilis study in May of 1997. “In order for America to reach its fullest potential, we must truly be one America … trusting each other, caring for each other,” Shaw said during his speech.STEPHEN JAFFE/AFP via Getty Images
Addressing and dismantling the racism behind that unequal treatment “will require changing systems, laws, policies and practices,” researchers wrote in Health Affairs in February. Those changes should include mandating standards for health care systems to achieve equitable results for patients, and medical training in the health effects of structural racism, knowledge that would be required for professional licensing, Hardeman and colleagues wrote in 2020.
Some medical schools are bolstering their curriculum with more extensive instruction on racism and health inequities.
Doriane Miller, a primary care physician at the University of Chicago Pritzker School of Medicine and director of the institution’s Center for Community Health and Vitality, leads doctors in training on tours of the surrounding area, in the south side of Chicago. People often see the area as defined by poverty and violence, Miller says. The tour offers a different story.
Miller talks about “how people came to this city looking for opportunities from the Deep South, in order to escape racism and segregation, and formed thriving businesses and communities.” She takes the new doctors by Provident Hospital, founded by the Black surgeon Daniel Hale Williams in 1891. The first Black-owned and -operated hospital in the nation, it also provided training for Black doctors and nurses. Williams performed the first successful open-heart surgery in the United States in 1893 and helped establish the National Medical Association, the first national organization of medical professionals open to African Americans.
The historical tour is a way to give new doctors “a sense of, not just physical place, but the people they will be serving,” Miller says. People “want to have you understand their circumstances, so that you can respond to them as individuals,” she says, “rather than making presumptions about who they are and where they come from.”
Like the presumptions many made about the men included in the syphilis study. “What happens is that the humanity and the individuality and the life experiences and history of the men themselves, and their families, are erased,” Northington Gamble says. “People forget the fact that these were men with lives and families and stories.”

