University of California, Los Angeles and University of California, San Diego researchers developed an injectable sealant for rapid hemostasis and tissue adhesion in soft, elastic organs.
Formulated with methacryloyl-modified human recombinant tropoelastin (MeTro) and Laponite silicate nanoplatelets (SNs), the engineered hydrogel demonstrated substantial improvements in tissue adhesion strength and hemostatic efficacy in preclinical models involving lung and arterial injuries.
Injuries to soft tissues such as lungs, heart, and blood vessels complicate surgical closure due to their constant motion and elasticity. Sutures, wires, and staples are mechanically fixed, risking blood loss when applied to tissues that expand and contract with each breath or heartbeat. Existing hemostatic agents, including fibrin-based sealants, aim to stem blood flow but may trigger intense coagulation responses in patients with clotting disorders.
Products like cyanoacrylates deliver strong adhesion yet introduce excessive stiffness that can disrupt natural tissue movement and cause cytotoxic effects. Natural polymer hydrogels are biocompatible but often lack the mechanical strength and adhesion needed for sealing wet or highly elastic surfaces. Progel and poly(ethylene glycol)-based FocalSeal demonstrate limited elasticity and require extended application times, reducing their effectiveness in dynamic tissue environments.
Soft tissue sealants that integrate hemostasis, flexibility, and adhesion remain limited. MeTro previously showed biocompatibility and mechanical properties resembling those of native elastic tissues.
Prior modifications with graphene oxide increased toughness, while methacryloyl-modified gelatin enhanced nerve repair. Hemostatic capabilities, however, remained a gap. SNs have the potential for improving clotting response while maintaining the sealant’s mechanical integrity.
In the study, “Rapid closure and hemostasis of ruptured soft tissues using a modified human tropoelastin-based sealant in preclinical models,” published in Science Translational Medicine, researchers conducted preclinical testing of an engineered hydrogel combining MeTro and Laponite SNs to assess tissue adhesion and hemostatic efficacy in soft tissues.
Preclinical testing involved arterial injury models in rat and lung injury in pig subjects to assess the sealant’s performance in soft, elastic organs. Researchers measured adhesion strength, clotting time, and tissue response to evaluate the effectiveness of the MeTro/SN formulation under dynamic physiological conditions.
Prepolymer solutions of MeTro and varying concentrations of SNs were prepared and cross-linked using visible light. Rat and pig subjects underwent injury procedures to assess the sealant’s efficacy.
Testing involved ex vivo adhesion strength measurements on pig skin, lung, and heart tissues, with burst pressure evaluated on punctured collagen sheets. Hemostatic performance was assessed through clotting time analysis using fresh human blood treated with MeTro/SN hydrogels and commercial hemostatic agents.
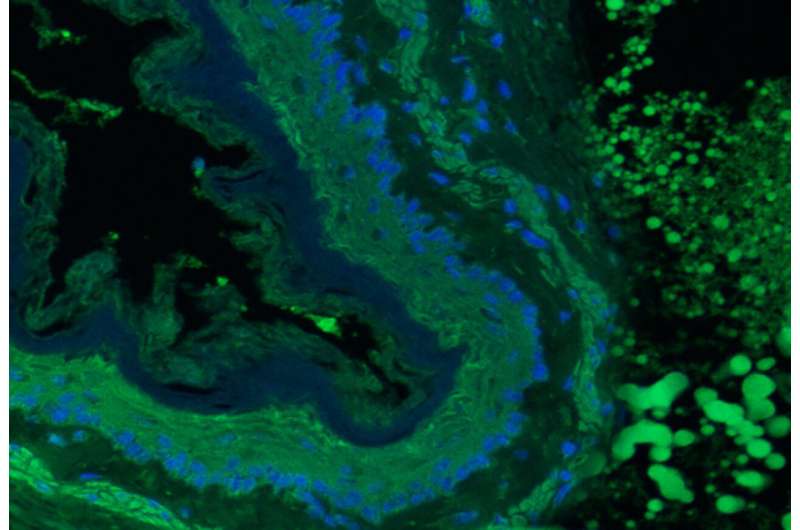
Biocompatibility assessments included live/dead staining and histological analysis of tissue surrounding MeTro/SN hydrogel implants. Additional testing included zeta potential analysis to evaluate electrostatic interactions and nuclear magnetic resonance spectroscopy to confirm cross-linking and chemical composition of the hydrogel matrix.
MeTro/SN hydrogels exhibited increased adhesion strength and burst pressure compared to MeTro alone and commercial sealants. On pig lung tissue, MeTro/SN achieved an adhesion strength of 23 kPa compared to 12 kPa for MeTro. Burst pressure of MeTro/SN hydrogels containing 1% SN reached 3.6 kPa, exceeding MeTro’s 2.8 kPa.
In ex vivo heart burst pressure tests, MeTro/SN tolerated pressures of 47 kPa compared to 41 kPa for MeTro, indicating improved structural integrity. Collagen-sheet burst pressure tests also showed superior mechanical strength in MeTro/SN-treated samples.
Hemostatic testing demonstrated reduced clotting time in MeTro/SN-treated samples compared to untreated controls. Blood treated with MeTro/SN hydrogels containing 1% SN clotted within 12 minutes, while untreated blood required 15 minutes. No increase in hemolysis was observed, indicating minimal cell damage despite the faster clotting response.
In the rat tail amputation model, MeTro/SN hydrogels reduced blood loss by approximately 91% compared to MeTro and by 99% compared to untreated controls.
Histological analysis revealed no significant inflammatory response surrounding MeTro/SN implants after seven and 28 days in rat subcutaneous tissue. No fibrosis or lymphocyte infiltration was observed, indicating biocompatibility of the hydrogel formulation.
In the pig lung injury model, MeTro/SN hydrogels maintained seal integrity and prevented blood loss for 14 days under physiological pressures. No significant detachment or tissue damage was observed during pressure testing, confirming the hydrogel’s adhesive stability in dynamic tissue environments.
Researchers conclude that MeTro/SN hydrogels provide effective sealing and hemostasis in soft, elastic tissues while maintaining biocompatibility in preclinical models. Improved adhesion strength and burst pressure on lung and arterial tissues indicate the potential for clinical application in traumatic injuries where conventional sealants fail to adhere under dynamic conditions.
Integration of SNs reduced clotting time without inducing inflammatory responses, supporting the hydrogel’s potential for rapid intervention in hemorrhagic wounds. Biocompatibility analysis demonstrated minimal immune response and tissue damage after implantation, suggesting a low-risk profile for clinical translation.
More information:
Mahsa Ghovvati et al, Rapid closure and hemostasis of ruptured soft tissues using a modified human tropoelastin-based sealant in preclinical models, Science Translational Medicine (2025). DOI: 10.1126/scitranslmed.adr6458
© 2025 Science X Network
Citation:
Better than stitches: Researchers develop biocompatible patch for soft organ injuries (2025, May 17)
retrieved 17 May 2025
from https://medicalxpress.com/news/2025-05-biocompatible-patch-soft-injuries.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.

