It is not every day that drug development results in a breakthrough with the potential to eliminate an often serious and sometimes fatal disease, but one of those days occurred earlier this month.
Earlier this month, the FDA approved a vaccine against respiratory syncytial virus (RSV) for the prevention of lower respiratory tract disease caused by the virus in individuals 60 years of age and older. It is the first RSV vaccine to gain approval anywhere in the world. It was a long haul and is a hugely important development.
RSV is a common respiratory virus and the most common cause of bronchiolitis (inflammation and swelling of the small airways in the lung) and pneumonia (infection of the lung tissue itself) in children younger than 1 year of age in the United States. Almost all children get an RSV infection by the time they are 2. Most of the time it causes a mild, cold-like illness, but it can be dangerous for some infants and young children. Each year in the United States, an estimated 58,000-80,000 children younger than 5 years old are hospitalized due to RSV infection.
RSV can also be serious in people with weakened immune systems and in older adults with underlying heart or lung conditions. In people in that demographic, RSV commonly affects the lower respiratory tract and can cause life-threatening bronchiolitis and pneumonia. According to the Centers for Disease Control, each year in the U.S., RSV leads to approximately 60,000-120,000 hospitalizations and 6,000-10,000 deaths among adults 65 years of age and older.
The FDA approved GSK’s RSV vaccine (brand name, “Arexvy”) on the basis of Phase III clinical-trial data from 25,000 subjects aged 60 or older that were published in The New England Journal of Medicine in February. In that study, a single shot of the vaccine reduced the risk of lower respiratory tract disease from RSV by 82.6% and of developing severe disease by 94.1%. Participants will continue to be studied through three RSV seasons to assess the duration of effectiveness and the safety and effectiveness of repeat vaccination. (Only data for the initial dose of Arexvy from the first RSV season of the study were available for the FDA evaluation.)
With respect to safety, as expected there were more adverse events with the vaccine than with placebo, but most reported adverse events were transient, with mild-to-moderate severity. The most frequent side effects were pain at the injection site, fatigue, muscle pain, headache, and joint stiffness or pain. The FDA concluded that there was sufficient evidence that the vaccine was safe and effective for approval.
There will likely be other RSV vaccines available soon: Pfizer and Moderna also have their own versions under FDA review for people aged 60 or above, and clinical trials have been completed in pregnant women, with the expectation that their maternal antibodies will protect their newborns.
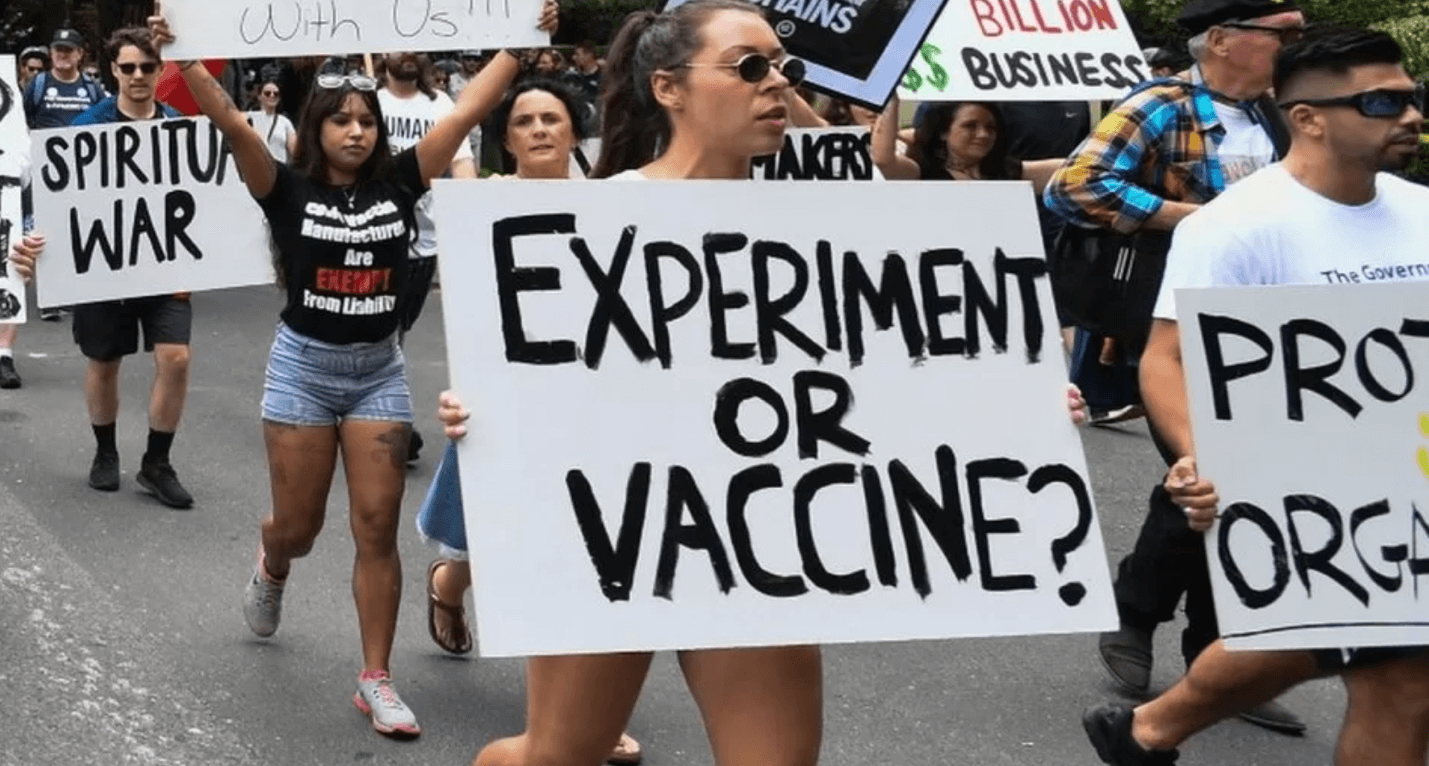
Unfortunately, public sentiment toward vaccines in general has been negatively affected by anti-vaccine activists who have spread disinformation relentlessly during the COVID-19 pandemic and before that about childhood vaccines.
Vaccines are now an ideological issue on the left and right. Presidential candidate Robert F. Kennedy, Jr., a Democrat, has targeted both, as has the Organic Consumers Association. Other activists intend to broaden their attacks on vaccines.
To encourage high uptake of this RSV vaccine (and others, which are reportedly nearing FDA approval), there is a need for an intensive public-private effort by public health officials, politicians, celebrities, and commentators of every stripe to get the word out. Let us not forget that vaccines don’t save lives; vaccinations do.
Henry I. Miller, a physician and molecular biologist, is the Glenn Swogger Distinguished Fellow at the American Council on Science and Health. He was the founding director of the FDA’s Office of Biotechnology. Find Henry on Twitter @HenryIMiller

