Listen to this story about long COVID realities
Click here for a full audio version of this story, read by Science News staff writer Meghan Rosen.
Audio: M. Rosen, H. Thompson
Belinda Hankins first grappled with COVID-19 in the spring of 2020. She had a fever, chills and trouble breathing, but the real clincher was her loss of smell. Hankins remembers opening a canister of Tony Chachere’s creole seasoning, lowering her nose to take a whiff, and not smelling a thing. “That stuff usually clears the kitchen,” she says.
Her second infection, two years later, was worse. After 12 long weeks of endless fatigue and aching joints, her doctor suggested she seek treatment for long COVID. The lingering, sometimes full-body condition can plague people for months or years after a COVID-19 infection (SN Online: 7/29/22).
In late August, I joined Hankins, age 64, in a small exam room for her first in-person consultation at the Johns Hopkins Post-Acute COVID-19 Team clinic. Wearing a navy dress and a blue surgical mask, Hankins is sitting in a chair across from physician Alba Azola. As they discuss Hankins’ symptoms, doctor and patient face each other, Azola occasionally swiveling her stool to tap notes into a computer.
Hankins’ symptoms are extensive. Brain fog, fatigue and pain top the list. She’s depressed. Sleep doesn’t feel restful. She has trouble focusing, is often light-headed and regularly loses her balance. Even walking to the clinic from the parking lot left her winded and in pain. “I’m extremely exhausted,” she says. “I have not felt good in a long time.” Hankins, pauses, wiping away a tear. “I wasn’t like this before.”
A life upended
Listen to Belinda Hankins describe her experience with long COVID in this short clip.
Audio: M. Rosen
Hankins, a retired digital media consultant, used to be an avid skier and a cyclist. She loved to travel and dance and was planning to learn how to play golf. She’s not sure what the future holds, though she tells me she still has faith she can be active again.
Treating people with long COVID can be complicated – especially for Hankins and those who have other medical conditions. She has pulmonary hypertension, fibromyalgia and the connective tissue disease scleroderma. It’s tricky to tease out which symptoms come from the viral infection. Azola’s approach is to listen, ask questions and listen some more. Then, she’ll zero in on a patient’s most pressing concerns. Her goal: manage their symptoms. “How can we make their quality of life better?” she asks.
 Belinda Hankins has been experiencing long COVID symptoms for months.B. Hankins
Belinda Hankins has been experiencing long COVID symptoms for months.B. Hankins
System overload
On the afternoon of Hankins’ visit, it’s a warm summer day in Baltimore, blue skies laden with fleecy clouds. Inside the labyrinthine halls of Johns Hopkins Bayview Medical Center, the vibe is not quite as sunny: bright lights, shiny floors, people in line and people in scrubs. Everyone I see is masked.
Azola meets me in the waiting area, walking briskly and wearing bright red glasses. Before the pandemic, Azola, a rehabilitation physician, treated patients recovering from strokes, spinal cord injuries and other disorders. Most mornings, she still works with these patients. But for the past two years, her afternoons have been booked with people laid low by COVID-19.
She’s squeezed me in to talk about the Johns Hopkins PACT clinic, which opened in April 2020, around the time when the world hit one million confirmed cases. “To be honest, we didn’t know what to expect,” Azola says. Back then, most of the clinic’s patients were recovering from COVID-19 after a stay in the hospital’s intensive care unit. Now, at least half of their patients never got sick enough with COVID-19 to be hospitalized – yet still had symptoms they couldn’t shake. In a single week, Azola and her colleagues may get 30 referrals. “It’s constant,” she says, “more than we can provide service to.”
As those referrals pile up, patient wait times can stretch. The PACT clinic expanded last summer, and now has more than a dozen people on staff, including therapists, physicians and other specialists. They try to keep the wait to around two months, Azola says, but sometimes it takes up to four months for a patient to be seen.
 Alba Azola (left), a rehabilitation physician at Johns Hopkins Medicine, focuses on managing the symptoms of her patients with long COVID.JOHNS HOPKINS POST-ACUTE COVID-19 TEAM (PACT)
Alba Azola (left), a rehabilitation physician at Johns Hopkins Medicine, focuses on managing the symptoms of her patients with long COVID.JOHNS HOPKINS POST-ACUTE COVID-19 TEAM (PACT)
The demand here and at clinics across the country isn’t likely to let up. As of mid-November, the United States has reported nearly 97.9 million cases of COVID-19. Though long COVID numbers can be hard to pin down, nearly half of people infected with SARS-CoV-2 hadn’t fully recovered six to 18 months after their infection, according to a large Scottish study published in Nature Communications on October 12. A more conservative estimate from the United States suggests that more than 18 million U.S. adults could have long COVID.
“We are in the middle of a mass disabling event,” says Talya Fleming, a physician at the JFK Johnson Rehabilitation Institute in Edison, N.J.
Scattershot solutions
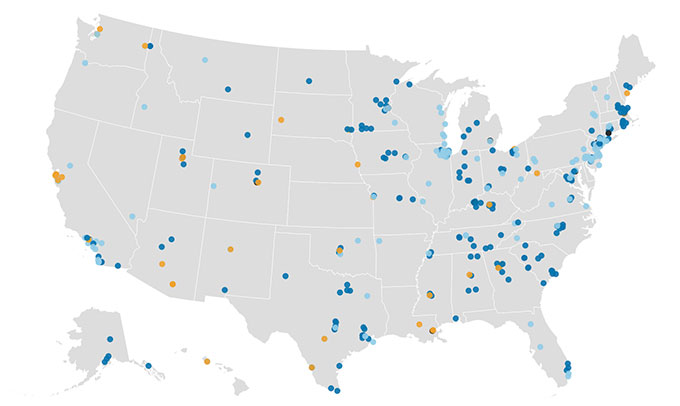
In the United States, some 400 clinics have popped up from coast-to-coast to care for the growing wave of long COVID patients.
Although the American Academy of Physical Medicine and Rehabilitation has published some guidance, no gold-standard therapies exist and there are no formal criteria for long COVID clinic performance. The Academy brought together more than 40 post-COVID clinics, including the Hopkins PACT clinic, to share experiences and discuss best practices for long COVID treatment. “We’re kind of guiding each other,” Azola says. Other clinics in the United States are more-or-less forging their own paths.
Today, Azola and colleagues are focusing on their patients’ symptoms, a strategy other long COVID doctors and clinics are using too. “There is no one, singular long COVID experience,” says pulmonologist Lekshmi Santhosh. So doctors really need to take a “customized, symptom-directed approach.”
Santhosh founded the OPTIMAL clinic at the University of California, San Francisco to provide follow-up care for people who had COVID-19. Since 2020, she’s seen hundreds of patients, who can wait weeks to months for an appointment, like they do at Hopkins. One main question Santhosh hears from patients is: “When am I going to get better?” That’s hard to answer, she admits.
General Symptoms

- Fatigue that interferes with daily life
- Symptoms that get worse after physical or mental effort (also known as post-exertional malaise)
- Fever
- Joint or muscle pain
- Rash
- Changes in menstrual cycles
Lungs and Heart

- Difficulty breathing or shortness of breath
- Cough
- Chest pain
- Fast-beating or pounding heart
Brain

- Difficulty thinking/
Brain fog - Headache
- Sleep problems
- Dizziness when standing up
- Pins-and-needles feelings
- Change in smell or taste
- Depression or anxiety
Gut

- Diarrhea
- Stomach pain
Scientists can’t yet predict how or when a patient will recover, and they don’t know why long COVID strikes some people and spares others. Right now, there are no obvious rules. “If you are young, you can get long COVID. If you have no pre-existing health conditions, you can get long COVID. If you’ve had COVID before, you still can get long COVID,” Fleming says. The list goes on.
At UCSF, Santhosh says she’s seen it all. Long COVID can affect a 75-year-old patient who was hospitalized for COVID-19, or a 35-year-old marathoner whose stubborn symptoms developed after just a mild infection. One patient can be hit with a hailstorm of health conditions, another patient, just a few.
“I’ve heard some weird things,” Azola says. She remembers one patient who felt as if a phone were vibrating deep inside their bones. Another described a sensation of heaviness, like their legs were made of lead.
Long COVID’s scattershot symptoms currently require a smorgasbord of solutions. For headaches, a doctor might prescribe a combo of pain relievers. For shortness of breath, an inhaler to open the airways could help. For brain fog, patients might visit a therapist who can help them with word-finding issues. Such symptom management is necessary, Azola says, because “we don’t have strong, randomized controlled trials to support the use of specific medications or treatments,” she says.
Developing effective therapies has been “frustratingly slow,” Santhosh says. Scientists are still trying to understand what’s happening in the body that spurs long COVID and lets symptoms simmer away unchecked. “The underlying biology is unclear,” she says. That makes it “unclear exactly what treatments might work.”
Long COVID’s biological underpinnings are a hot topic among researchers today, says Mike VanElzakker, a neuroscientist at Harvard Medical School and Massachusetts General Hospital, and part of the Long COVID Research Initiative, a group working to study and treat the condition. Scientists have scads of hypotheses for what causes long COVID symptoms, including lungs scarred by SARS-CoV-2 or the reawakening of some other, long-slumbering virus. One idea posits that COVID-19 might sabotage the immune system, inviting other microbes to do harm. Another idea pins long COVID on caches of coronavirus hiding within the body’s tissues.
“It really does matter what’s causing these problems,” VanElzakker says. If doctors knew what’s driving a patient’s symptoms, they might be able to offer personalized treatments aimed at the illness’s root.
Filling the void
On Facebook pages and websites around the internet, purported long COVID treatment options abound.
Vitamins, supplements, alternative medicines: general internist Aileen Chang in Washington, D.C. used to hear all the time from long COVID patients about therapies they’ve tried. In the fall of 2020, Chang and colleagues started the George Washington Medical Faculty Associates COVID-19 Recovery Clinic, which later closed its doors due to a staffing shortage. She recalls patients who flew to different countries to have their blood filtered and others who took “every sort of supplement you can imagine,” she says. “They’re looking for solutions.”
Without clear data on what long COVID treatments work, opportunists have stepped in to fill the void. Some unproven treatments may be scams with serious side effects; they can also drain patients financially. “They’re spending all this money on things they think will make them better,” Chang says, “but the truth is… we don’t know.”
What scientists do know is that potential long COVID treatments are still in their early days. There’s some evidence that getting a COVID-19 vaccine can improve long COVID patients’ symptoms, though this idea is still controversial, researchers reported in November in eClinicalMedicine. And repeated sessions of breathing 100 percent oxygen in a hyperbaric chamber might relieve fatigue and brain fog, small studies of patients have suggested.
See all our coverage of the coronavirus pandemic
Last year, the U.S. National Institutes of Health launched a massive research project on the long-term effects of COVID-19. Called the RECOVER Initiative, the project aims to uncover why some people get long COVID and to identify underlying causes. As of November 11, RECOVER has enrolled 10,645 of an estimated 17,680 adults needed.
It’s a great initiative, Santhosh says, but it got rolling relatively late – well after long COVID had already upended many people’s lives. “We need… a lot more funding and a lot more therapeutic trials,” she says. Santhosh is hopeful that, in the coming months and years, doctors will have solid answers on what treatments actually work. “There are a lot of tantalizing biological leads,” she says. Though she knows that this timeframe can feel agonizingly long to patients and clinicians.
Where are the long covid clinics?
For people with long COVID, finding a place to get appropriate medical care is a challenge. Read more and explore our interactive maps.
Real life
In the meantime, Santhosh, Azola and other physicians are borrowing strategies that help for other disorders – like myalgic encephalomyelitis/chronic fatigue syndrome. Many of the symptoms of that still-mysterious illness overlap with those of long COVID, a symmetry that could bring answers for both disorders, scientists suggest September 8 in Science.
One common approach isn’t a treatment like pills or surgery, it’s more of a shift in behavior: Don’t overdo it, Santhosh says. “We talk to our long COVID patients about this all the time, about the need to rest, to pace yourself and how to gently bring back your aerobic fitness.”
Long COVID patients with fatigue can be tempted to try and push through, to keep speeding through life as they had before their diagnosis. But that doesn’t seem to work for people with chronic fatigue, and “for some long COVID patients, it can actually make things worse,” she’s found.
Azola has similar advice for Hankins. About a half hour into the appointment, Azola slides away from the computer desk, and turns toward her patient. “This is the part where people want to punch me in the face,” she tells Hankins, pushing her glasses up onto her head. “We don’t have a magic wand that makes [you] feel better.”
Instead, Hankins will need to check her body’s battery every day, conserve energy where she can, and build in opportunities to recover. Little tricks, like sitting in a chair while showering or prepping food, can help patients save enough juice to make it through the day. Azola hopes to get Hankins off the “corona coaster,” where patients can feel relatively good one day, and the next day, crash. Having energy levels constantly crater can erode a patient’s ability to live their lives, she says.
Staying hopeful
In this short clip, Belinda Hankins looks to the future.
Audio: M. Rosen
For the next 20 minutes, doctor and patient talk about how Hankins’ life has changed and what her next steps will be. In a week, she’ll meet with a neuropsychologist who will help her cope with her new reality; Azola also refers Hankins to a pain specialist.
The two women have spent about an hour together – a near-eternity for a medical appointment. For Azola, it’s time well spent. “The most important thing is to listen to patients and keep an open mind,” she says.
When I speak with Hankins nearly three weeks later, she’s still feeling hopeful. She’s met with the neuropsychologist, and will continue to receive follow-up care. For Hankins, a care plan that factors in all of her conditions, including long COVID, may one day let her feel like herself again.
For now, she’s hoping that sharing her story will help others struggling with the illness. When she tells people she has long COVID, she says, “some of them don’t even think it’s real.”

