Researchers from RWJBarnabas Health and Rutgers Cancer Institute, New Jersey’s only National Cancer Institute-designated Comprehensive Cancer Center, as well as Tufts Medical Center and The University of Manchester, have developed and validated the first individualized risk prediction model for adults diagnosed with early-stage classic Hodgkin’s lymphoma.
Known as the Early-stage Hodgkin International Prognostication Index (E-HIPI), the model estimates two-year progression-free survival (PFS) and is designed to support more personalized treatment planning for clinicians and patients.
The findings were published in NEJM Evidence and presented concurrently by co-first and corresponding author, Andrew M. Evens, DO, MBA, MSc, Deputy Director for Clinical Services for the Rutgers Cancer Institute and Chief Physician Officer of the Jack & Sheryl Morris Cancer Center, during the 18th International Conference on Malignant Lymphoma (ICML), a leading global forum for lymphoma research and clinical advancements.
The E-HIPI model was developed using data from over 3,000 adult patients enrolled in four, pivotal international phase III clinical trials. To ensure its accuracy, it was tested and validated in two real-world registry cohorts that included more than 2,300 people with early-stage classic Hodgkin’s lymphoma.
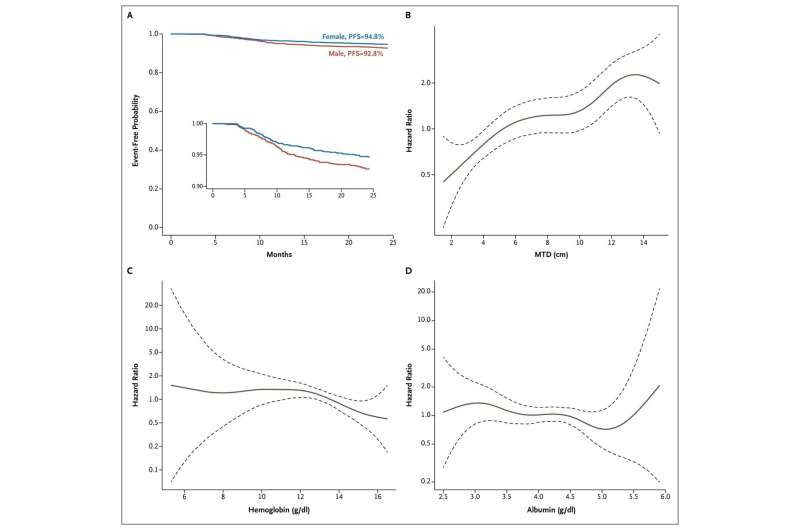
The model uses routinely available and objective clinical measures—like patient sex, tumor size, and exact values of common lab results such as hemoglobin and albumin levels—to help predict an individual patient’s chance of staying cancer-free for two years.
“Early-stage classic Hodgkin’s lymphoma is a highly curable cancer, particularly among young adults. However, despite high survival rates and significant advances in treatment, we’ve lacked a validated tool to assess outcomes and estimate a patient’s individual risk of relapse,” said Dr. Evens, who is also System Director of Medical Oncology and Oncology Lead, RWJBarnabas Health Medical Group, Associate Vice Chancellor for Clinical Innovation and Data Analytics at Rutgers Biomedical and Health Sciences.
“Through this global collaboration with researchers at Tufts Medical Center, the University of Manchester in the United Kingdom, and all our international partners, we developed a robust, dynamic, and data-driven model that leverages common clinical variables to generate more precise predictive insights.
“This tool has the potential to enhance clinical decision-making, personalize treatment strategies, and ultimately improve long-term outcomes for patients worldwide.”
The E-HIPI model demonstrated strong and consistent performance across all datasets and outperformed the widely used European Organization for Research and Treatment of Cancer (EORTC) favorable/unfavorable classification.
To facilitate real-world implementation, the research team developed interactive online risk calculators, to support shared decision-making between clinicians and patients. In addition to informing about personalized treatment, the E-HIPI provides modernized risk stratification for the design of future clinical trials and research studies.
“We hope that this model will enhance communication between patients and clinicians, and promote a greater understanding of the short- and long-term risks and benefits of different treatment options for early-stage classic Hodgkin’s lymphoma,” said Susan K. Parsons, MD, MRP, medical director of the adolescent and young adult (AYA) cancer survivorship program, research director of the Center for Health Solutions at Tufts Medical Center, co-founder of the HoLISTIC Consortium, and co-senior author of the study.
“Ideally, this type of information about treatment trade-offs will alleviate some of the burden experienced in the cancer journey.”
“We rigorously developed and validated our model based on an established checklist for predictive modeling,” said Angie Mae Rodday, Ph.D., investigator in the Institute for Clinical Research and Health Policy Studies at Tufts Medical Center, biostatistician at the Tufts Clinical and Translational Science Institute and lead statistician for the project.
“When we compared our model to existing classification systems, it had better performance and was more strongly related to patient outcomes. The online calculator we developed as a result of this work is accurate, accessible, easy-to-use and is completely free for patients and clinicians.”
This research was made possible through the HoLISTIC (Hodgkin Lymphoma International Study for Individual Care) Consortium, a global effort combining data from seminal randomized clinical trials and cancer registries, which are enriched with long-term patient follow-up.
Rachel Murphy-Banks, program manager of the Reid R. Sacco Adolescent & Young Adult Cancer Program at Tufts Medical Center and project manager of the HoLISTIC Consortium, was a key contributor to the visualization of the graphic interface.
More information:
Angie Mae Rodday et al, An Individualized Prediction Model for Early-Stage Classic Hodgkin’s Lymphoma, NEJM Evidence (2025). DOI: 10.1056/EVIDoa2500115
Provided by
Rutgers Cancer Institute
Citation:
Risk prediction model offers personalized outlook for early-stage Hodgkin’s lymphoma (2025, June 20)
retrieved 20 June 2025
from https://medicalxpress.com/news/2025-06-personalized-outlook-early-stage-hodgkin.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.

