After World War II, Nuremberg, Germany, was the site of trials of Nazi officials charged with war crimes and crimes against humanity. The Nuremberg trials were landmarks in the development of international law. But one of them has also been applied in peacetime: the “Medical Trial,” which has helped to shape bioethics ever since.
Twenty Nazi physicians and three administrators were tried for committing lethal and torturous human experimentation, including freezing prisoners in ice water and subjecting them to simulated high-altitude experiments. Other Nazi experiments included infecting prisoners with malaria, typhus and poisons and subjecting them to mustard gas and sterilization. These criminal experiments were conducted mostly in the concentration camps and often ended in the death of the subjects.
Lead prosecutor Telford Taylor, an American lawyer and general in the U.S. Army, argued that such deadly experiments were more accurately classified as murder and torture than anything related to the practice of medicine. A review of the evidence, including physician expert witnesses and testimony from camp survivors, led the judges to agree. The verdicts were handed down on Aug. 20, 1947.
As part of their judgment, the American judges drafted what has become known as The Nuremberg Code, which set forth key requirements for ethical treatment and medical research. The code has been widely recognized for, among other things, being the first major articulation of the doctrine of informed consent. Yet its guidelines may not be enough to protect humans against new potentially “species-endangering” research today.
10 key values
The code consists of 10 principles that the judges ruled must be followed as both a matter of medical ethics and a matter of international human rights law.
The first and most famous sentence stands out: “The voluntary consent of the human subject is absolutely essential.”
In addition to voluntary and informed consent, the code also requires that subjects have a right to withdraw from an experiment at any time. The other provisions are designed to protect the health of the subjects, including that the research must be done only by a qualified investigator, follow sound science, be based on preliminary research on animals and ensure adequate health and safety protection of subjects.
The trial’s prosecutors, physicians and judges formulated the code by working together. As they did, they also set the early agenda for a new field: bioethics. The guidelines also describe a scientist-subject relationship that obligates researchers to do more than act in what they think is the best interests of subjects, but to respect the subject’s human rights and protect their welfare. These rules essentially replace the paternalistic model of the Hippocratic oath with a human rights approach.
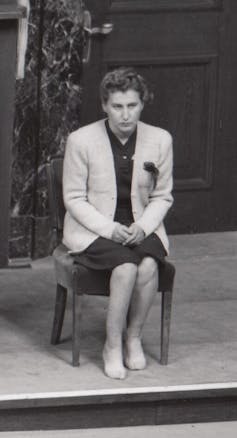
United States Holocaust Memorial Museum via Wikimedia Commons
Under President Dwight D. Eisenhower, who had been the commanding general in Europe, the U.S. Department of Defense adopted the code’s principles in 1953 – one sign of its influence. Its fundamental consent principle is also summarized in the U.N.’s International Covenant on Civil and Political Rights, which declares that “no one shall be subjected without his free consent to medical or scientific experimentation.”
Yet some physicians tried to distance themselves from the Nuremberg Code because its source was judicial rather than medical, and because they did not want to be linked in any way to the Nazi physicians on trial at Nuremberg.
The World Medical Association, a physicians group set up after the Nuremberg Doctors Trial, formulated its own set of ethical guidelines, named the “Helsinki Declaration.” As with Hippocrates, Helsinki permitted exceptions to informed consent, such as when the physician-researcher thought that silence was in the best medical interest of the subject.
The Nuremberg Code was written by judges to be applied in the courtroom. Helinski was written by physicians for physicians.
There have been no subsequent international trials on human experimentation since Nuremberg, even in the International Criminal Court, so the text of the Nuremberg Code remains unchanged.
New research, new procedures?
The code has been a major focus of my work on health law and bioethics, and I spoke in Nuremberg on its 50th and 75th anniversaries, at conferences sponsored by the International Physicians for the Prevention of Nuclear War. Both events celebrated the Nuremberg Code as a human rights proclamation.
Office of Military Government for Germany (U.S.) via Wikimedia Commons
I remain a strong supporter of the Nuremberg Code and believe that following its precepts is both an ethical and a legal obligation of physician researchers. Yet the public can’t expect Nuremberg to protect it against all types of scientific research or weapons development.
Soon after the U.S. dropped atomic bombs over Hiroshima and Nagasaki – two years before the Nuremberg trials began – it became evident that our species was capable of destroying ourselves.
Nuclear weapons are only one example. Most recently, international debate has focused on new potential pandemics, but also on “gain-of-function” research, which sometimes adds lethality to an existing bacteria or virus to make it more dangerous. The goal is not to harm humans but rather to try to develop a protective countermeasure. The danger, of course, is that a super harmful agent “escapes” from the laboratory before such a countermeasure can be developed.
I agree with the critics who argue that at least some gain-of-function research is so dangerous to our species that it should be outlawed altogether. Innovations in artificial intelligence and climate engineering could also pose lethal dangers to all humans, not just some humans. Our next question is who gets to decide whether species-endangering research should be done, and on what basis?
I believe that species-endangering research should require multinational, democratic debate and approval. Such a mechanism would be one way to make the survival of our own endangered species more likely – and ensure we are able to celebrate the 100th anniversary of the Nuremberg Code.

