The life and political legacy of former Vice President Dick Cheney, who died on Nov. 4, 2025, at the age of 84, has been well documented. But his decades-long battle with heart disease may be less appreciated.
Cheney benefited from almost every major advance made in cardiovascular medicine. These breakthroughs enabled him to sustain an active political career and gave him additional years of an enjoyable life after he moved away from the political spotlight.
As a cardiologist who specializes in both sports medicine and heart disease, as well as advanced heart failure and transplant cardiology, I frequently provide care for patients who, like Cheney, are supported by powerful medicines and procedures to help support heart function.
Cheney’s passing provides an opportunity to reflect on the rapid evolution in medical technology, especially in the past half-century, that improved the lifespan and overall quality of life for Cheney, as well as millions of heart patients around the world.
Mario Tama/Hulton Archive via Getty Images
The formative days of cardiac medicine
Cheney suffered his first of five heart attacks at age 37, in 1978, when the standard of care mainly involved pain relief and bed rest, and when medical professionals did not yet have a clear understanding of what causes heart attacks in the first place.
Today, doctors understand that a heart attack occurs when blood flow through an artery is blocked by a blood clot called a thrombus and oxygen cannot get to the heart muscle. Imagine a kink in a hose that prevents water passing through it. When the heart muscle does not receive oxygen for a long enough period of time, the heart muscle will die and a scar will form.
In the 1960s and ’70s, however, doctors thought a thrombus was the result of – not the cause of – a heart attack.
It is now clear that the formation of a thrombus leads to a heart attack rather than the other way around. That important lesson revolutionized the way doctors like me treat patients with heart attacks.
Eugene Mymrin/Moment via Getty Images
Big and small breakthroughs
Today, we reopen arteries with stents. When stents are not available, we use powerful medications called thrombolytics, or clot-busters, to break down the thrombus. These kinds of treatments seem commonplace today, but it wasn’t until 1988 that a pivotal study showed combining aspirin and streptokinase, a clot-buster drug, improved survival after a heart attack by almost 50%.
Cheney had additional heart attacks in 1984, 1988, 2000 and 2010. Notably, all but the last were during election years, underscoring the detrimental effects of stress on heart health. His heart attack in 2000 occurred as the courts worked to determine whether Al Gore or George W. Bush – with whom Cheney would become vice president – had won the presidential election.
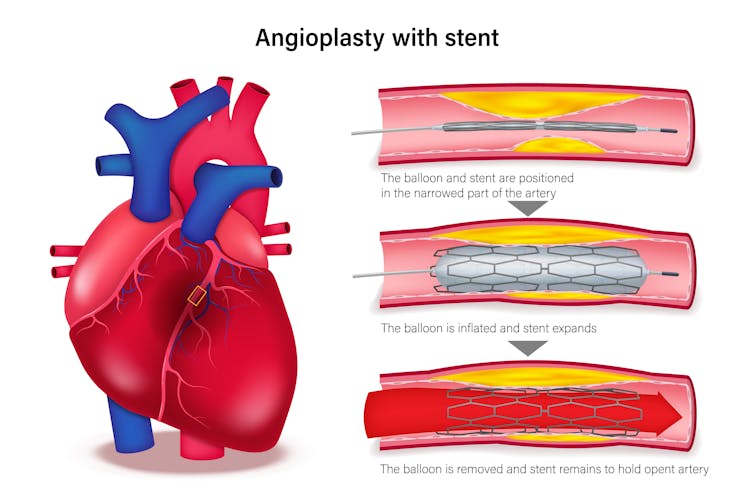
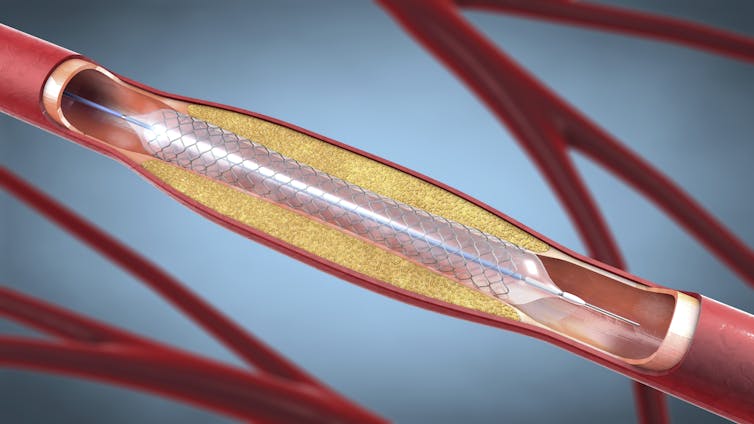
As technology advanced over the years, Cheney had multiple angioplasties – a procedure to open up narrowed or blocked arteries. During an angioplasty, a procedure developed in the 1980s, heart doctors would place a balloon made of flexible polymers inside an artery to open up and clear the thrombus.
While angioplasties were helpful, one of the main limitations was that the walls of the artery would quickly shrink back – known as recoiling – after the balloon was deflated.
Rujirat Boonyong/iStock via Getty Images Plus
How stents became mainstream
That limitation led to the concept of stents – devices that are now frequently used to treat heart attack patients.
Cheney’s first heart attack in 1978 occurred well before the first stents became available.
Stents started out as metal, tubelike structures that cardiologists used to open up narrowed or blocked blood vessels. The original stents, made of stainless steel, fixed the problem of blood vessels recoiling.
But over time, cardiologists found that stents become stenotic, meaning they themselves would become narrow, making it difficult for blood to flow through them. This problem was solved with the introduction of drug-eluting stents, which have a polymer that coats the metal struts of a stent and prevents stenosis from occurring.
Drug-eluting stents were a game-changer and reduced the need for repeated procedures by about 50% to 70%. Like millions of Americans, Cheney received several stents during his long battle with heart disease.
While stents are helpful, sometimes patients require a surgery called coronary artery bypass graft. Heart surgeons perform this procedure when there are blockages that angioplasty or a stent cannot fix, or when there are too many blockages in the heart arteries.
In 1988, at age 47, Cheney underwent a quadruple bypass operation to help restore blood flow to his heart following his third heart attack.
Christoph Burgstedt/Science Photo Library via Getty Images
Battling heart disease
Despite the best efforts of cardiologists, many patients with heart disease, like Cheney, go on to develop heart failure.
There are two main types of heart failure. One – called heart failure with preserved ejection fraction – occurs when the left ventricle, the largest and strongest chamber of the heart, becomes stiff and unable to relax.
The other type – heart failure with reduced ejection fraction – occurs when the left ventricle becomes enlarged and weakened, and fails to pump blood efficiently.
Both types of heart failure make it difficult for the heart to adequately pump blood throughout the body. Cheney, like millions of people throughout the world, suffered from a dilated and weakened heart.
Fortunately, now there are several classes of medications used to treat the kind of heart failure that Cheney suffered from.
There are four main types of drugs that heart failure cardiologists use to manage patients with this condition, which are referred to as the “four pillars” of heart failure management. These medications work together to reduce the amount of stress placed on the heart and to create an environment that helps a weakened heart pump blood more efficiently throughout the body.
Thanks to these four medication types, millions of patients with dilated, weak hearts are living much longer with a higher quality of life and staying out of the hospital. Some of these medications are also used for patients with stiffened hearts, but there is a lot of ongoing research to better understand how to take care of patients with that kind of heart failure.
Despite the use of medications to treat dilated, weak hearts, some patients suffer from continued weakening of the heart muscle and progress to end-stage, or advanced, heart failure. When this happens, there are only two treatment options available. These options are a mechanical pump or a heart transplant.
Heart transplantation is the gold-standard, preferred treatment option for advanced heart failure that results from a dilated, weakened heart.
In 2023, there were about 4,500 heart transplants in the U.S. and about 2,200 in Europe. On average, patients live well over a decade with a heart transplant, and many will go on to live for 20 to 30 more years.

Halfpoint Images/Moment via Getty Images
An ounce of prevention is worth a pound of cure
Benjamin Franklin famously quipped, “An ounce of prevention is worth a pound of cure.”
In an interview with “60 Minutes” in 2013, Cheney said his heart disease was the result of genetics and an unhealthy lifestyle. He admitted that he drank beer, ate fatty foods and also smoked three packs of cigarettes per day.
Millions of people across the U.S. and Europe have a lifestyle that is similar to that of Cheney’s prior to his heart transplant. While heart patients benefit from medications, stents and surgeries, preventive strategies cannot be underestimated.
Almost all major health organizations, including the American Heart Association, American Cancer Society and the Department of Health and Human Services, recommend 150 minutes per week of moderate-intensity exercise.
This recommendation translates to a brisk walk about 30 minutes per day, five days per week. This level of exercise leads to large increases in survival and preservation of overall health throughout a lifetime.
While Cheney lived through five heart attacks, the goal for patients and their doctors is to avoid the first. Scientific advances in cardiology have led to a dramatic improvement in survival and quality of life for millions of people, but preventive measures are still by far the most effective lifesaving measure.

